The VT CFIDS Association, Inc.

dba: The Vermont CFIDS Association, Inc. a 501(c)3 private foundation. P.O.Box 3162, Burlington, VT 05408 U.S.A. 1-802-881-3821
September 16, 2008:

Rik Carlson (left) President of the Vermont CFIDS Association (Chronic Fatigue Immune Dysfunction Syndrome) received a check for the establishment of a medical student scholarship at the University of Vermont Medical School. The check was presented by Dr. Kenneth J. Friedman (right) of Pawlet, VT on behalf of P.A.N.D.O.R.A. (Patient Alliance for Neuroendocrineimmune Disorders and Organization for Research and Advocacy). Dr. Friedman serves on the Executive Board of Directors as Secretary and is also Chairman of the Public Policy Committee of P.A.N.D.O.R.A.
The award to the Vermont CFIDS Association was made in recognition of Dr. Friedman’s leadership and efforts to enhance Chronic Fatigue Syndrome (CFS) education in the State of Vermont. This award was made also to honor his contribution, commitment, and accomplishments on behalf of the national community. The scholarship is modeled after the program he created currently running in all three of New Jersey’s medical schools. Since most medical schools do not include CFS in their medical school curriculum, the scholarship program supplements medical student education so that physicians in training can obtain knowledge about this illness.
The CFS medical student scholarship program will be operational in the Spring of 2009 and will encourage medical students to research Chronic Fatigue Syndrome during the summer between their first and second years of medical school. The student who writes the best essay, as determined by an evaluation committee, wins the scholarship.
Dr. Friedman: “The medical student scholarship program is designed to supplement rather than compete with the medical school curriculum. By encouraging students to learn about CFS in the one summer that they are not involved in classes, we encourage a productive use of their time. P.A.N.D.O.R.A. will expand its award program to other states soon.”
The Vermont CFIDS Association is one of only three organizations selected nationally and was hand picked by P.A.N.D.O.R.A. for its outstanding efforts in educating the public, passing legislation to allocate monies for a physicians’ diagnosis and treatment manual for Chronic Fatigue Syndrome and helping direct those afflicted to the best resources for coping with and treating the symptoms of their illness.
CFS or CFIDS is estimated to debilitate between 1 and 4 million Americans, and creates an estimated $9 billion annual loss to the American economy. (Centers for Disease Control and Prevention (CDC). It strikes men, women and children of all races and social backgrounds. It is life long and a cure remains elusive due to its complexity. Among its main symptoms are "bone crushing" fatigue not alleviated by rest, cognitive impairment, "flu-like" symptoms with or without debilitating muscle pain, long-term respiratory infections, gastrointestinal disorders, and other progressive neurological impairments leading to disability and the destruction of family life.
The 5 year grant will be disbursed as follows: $1,050 for the first year of the award, $1,050 for the second year, $750 for the third year, $500 for the fourth year and $250 for the fifth year of the award. The intent of the gradually diminishing awards in subsequent years is to encourage the Vermont CFIDS Association to identify donors and benefactors who will sponsor the program in future years to ensure the program will remain successful.
The Vermont CFIDS Association is proud to be the first organization to be selected for this national scholarship award program.
About P.A.N.D.O.R.A.:
http://www.pandoranet.info/
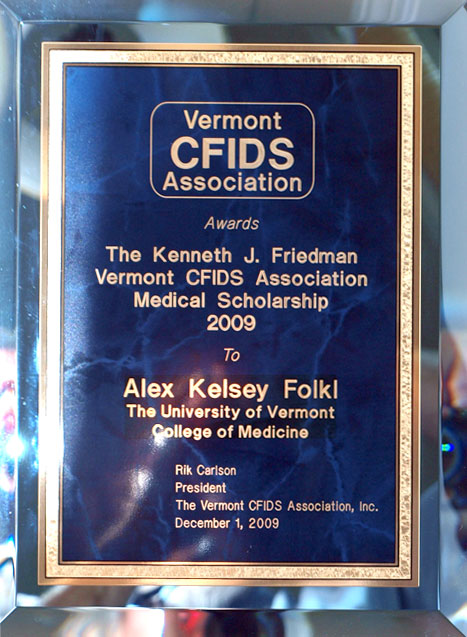
The Winner:
 |
Alex Folkl is the winner of the first annual Kenneth J. Friedman Vermont CFIDS Association Medical Scholarship Award. His essay can be seen here. He is from Toronto, Ontario, born in St. Louis, and his parents live in Detroit. He has a bachelors of science in biology and a masters in pathobiology from the University of Guelph (Ontario); and his wife, Kathryn, is an ecologist/program coordinator for the Nature Conservancy of Canada. Alex says, his opinion may change, but at the moment, he's interested in emergency or internal medicine, and spends most of his spare time rock climbing. In the northeast, that means the Adirondacks, Cannon Cliff, and Rumney, New Hampshire.
|
|---|

The Kenneth J. Friedman Vermont CFIDS Association Medical Scholarship Award
is presented to Alex Folkl on December 3, 2009.
The award winning essay can be seen Here
Write an essay of approximately 3,000 words on the following topic: Chronic Fatigue Immune Dysfunction
Syndrome (CFIDS) is a complex multi-system disorder. Describe the symptoms, diagnosis
and principals of treatment for CFIDS. Include in your answer a discussion of the differential diagnosis
of CFIDS from other illnesses with similar presentations.
Your essay must not exceed 10 double-spaced pages of 12-point type with 1-inch margins.
References should be cited within the text of the essay using standard, medical journal format.
At least 10 references should be cited.
A bibliography containing all references cited in the essay should be included at the end of the essay.
The bibliography should be formatted using standard, medical journal format.
The document needs to be scholarly and well-referenced. Citing web sites as references is not acceptable.
The essay must not have been offered or submitted elsewhere.
Essays not conforming to these standards will not be considered.
A committee has been formed by Vermont CFIDS Association to review the submitted essays and select
the winner. Judging will be on the basis of scholarship, and the demonstration of understanding the
difficulties involved in diagnosing and providing compassionate and effective care to CFS patients.
Chronic Fatigue Immune Dysfunction Syndrome: A Review (.pdf)
Chronic Fatigue Immune Dysfunction Syndrome: A Review
Abstract:
Chronic Fatigue Immune Dysfunction Syndrome (CFIDS) is a complex, multi-organ system disease of unknown etiology characterized by functionally debilitating exhaustion and a constellation of associated symptoms. Its diagnosis is complicated; its treatment is largely supportive; and full recovery is rare. As well, lack of medical acknowledgement of CFIDS as a legitimate disease has caused patients to suffer a significant social stigma. However, recent work characterizing improved CFIDS biomarkers coupled with a modified understanding of CFIDS etiology may foreshadow a transformation in the medical approach to this illness.
Symptoms and diagnosis of chronic fatigue immune dysfunction syndrome
The hallmark symptom of CFIDS is extreme chronic fatigue. In many cases, this follows a period of flu-like illness. However, no physical exam or laboratory finding is diagnostic of the disorder (Prins et al., 2006). Rather, its diagnosis is clinical and relies on the presence of symptomatic criteria outlined in one of several comparable case definitions (for example, the Oxford, London, or Centers for Disease Control [CDC] definitions). Of these, the CDC CFIDS criteria are the most widely employed (Prins et al., 2006). They are: 1) Debilitating, new-onset fatigue present for at least six months which is 2) not alleviated by rest and 3) results in a significant decrease in the ability to function normally in daily life, 4) accompanied by four or more of impaired memory or concentration, sore throat, tender cervical or axillary lymph nodes,
muscle or joint pain, new headaches, or post-exertional malaise, also present for six or more months (Fukuda et al., 1994).
Despite the availability of diagnostic criteria, a diagnosis of CFIDS is rarely straightforward. First, it is a diagnosis of exclusion. This is an unavoidable consequence of the lack of quantifiable, objective CFIDS biomarkers- yet the list of exclusionary criteria is substantial (Afari and Buchwald, 2003). Exclusionary criteria include fatigue caused by a known disease (a list of these would include hypothyroidism, anemia, diabetes, congestive heart failure, chronic obstructive pulmonary disease, kidney failure, adrenal insufficiency, cancer, autoimmune disease, certain medications, and persistent infection), fatigue caused by exertion, several psychiatric disorders including major depressive disorder, bipolar disorder, schizophrenia, dementia, delusional disorder, anorexia or bulimia, substance abuse, and severe obesity (Fukuda et al., 1994; Prins et al., 2006; Gonzales and Nadler, 2009). The time and cost of ruling these out can be quite significant. As well, the CFIDS diagnostic criteria may be incomplete. For example, a significant number of patients report gastrointestinal distress, dizziness, nausea, anorexia, night sweats, muscle fasciculations, sleep disturbances, and orthostatic hypotension in addition to their diagnostically-relevant symptoms. For some, these additional symptoms may be as distressing as those outlined as diagnostic criteria- making the initial presentation of CFIDS quite heterogeneous- yet they are not included in most case definitions (Afari and Buchwald, 2003; Janson et al., 2003; Prins et al., 2006). Finally, CFIDS criteria overlap significantly with those of several other syndromes, including fibromyalgia (unexplained chronic pain and fatigue), irritable bowel syndrome (unexplained gastrointestinal distress accompanied by psychiatric complaints), and others to such a degree that, in many patients, more than one of these diagnoses may
adequately explain all symptoms. In fact, some authors suggest these syndromes may actually be varying presentations of the same disease, such that which diagnosis a patient receives is largely dependent on which specialist does the diagnosing (Prins et al., 2006; Wessely et al., 1999). In an attempt to address these concerns, Carruthers et al., (2003) published an expanded clinical case definition that included such symptoms as sleep dysfunction and orthostatic hypotension; nonetheless, there continues to be considerable debate regarding the appropriate case definition of CFIDS (Prins et al., 2006), and as a result, the disorder may be significantly mis- or under-diagnosed.
Disagreement over the case definition of CFIDS coupled with its heterogeneous presentation and the complex, subjective nature of its diagnosis have made some physicians reluctant to accept it as a genuine physical illness. Instead, they suggest that it is entirely psychiatric in origin (Asbring and Narvanen, 2003; Gilje et al., 2008). (Interestingly, a group of general practitioners in Britain were far more dismissive of CFIDS than they were of irritable bowel syndrome, although, as noted above, the two may actually be varying presentations of the same disease [Raine et al., 2004]). Unfortunately, this skepticism has contributed to a significant social stigma: Its legitimacy disallowed by the medical profession, CFIDS has become a shameful secret for some- patients are accused of lying about their diagnosis or of using it to get out of commitments, and experience a significant amount of social isolation as a result (Asbring and Narvanen, 2002).
Despite its attendant controversy, the bulk of evidence indicates that CFIDS is a real, albeit, poorly-understood, physical disease entity. Not least among this evidence is the observation that experience of CFIDS can be entirely disabling for some patients.
The illness experience
CFIDS symptoms can cause significant problems in daily life. For example, as a result of fatigue, memory loss, and impaired concentration, patients have trouble interacting with others and experience strained relationships with families, friends, and significant others (indeed, many CFIDS patients may end or avoid romantic relationships, fearing an inability to fulfill the expectations of another person) (Travers and Lawler, 2008; Anderson and Ferrans, 1997; Arrolls and Senior, 2008). As well, many experience difficulty with mobility and with common activities of daily living such as food preparation and housekeeping (Arrolls and Senior, 2008). About two-thirds find it difficult to maintain full-time employment and lose substantial income and accumulate significant debt as a result or their illness (Afari and Buchwald, 2003; Buchwald et al., 1996; Edwards et al., 2007). Perhaps most devastating, many CFIDS patients experience a significant burden of mental illness as a result of their disease: A loss of self as symptoms curtail access to activities of their former lives; a feeling of isolation from society at large; and the indignity of living with a medically-stigmatized disease (Travers and Lawler, 2008). Unsurprisingly, depression is common in the CFIDS community (Priebe et al., 2008). Yet the experience of CFIDS is not uniform. For example, fatigue onset in some individuals is gradual, while in others, it is abrupt, and in most individuals symptoms come and go unpredictably and with varying degrees of severity (Afari and Buchwald, 2003; Anderson and Ferrans, 1997).
Etiology, treatment and prognosis
With the exception of several complementary approaches (for example, fatty acid supplementation, osteopathy, homeopathy, and acupuncture, none of which has been shown to be effective), CFIDS treatments have largely been designed to mitigate the supposed causes of the disorder [Whiting et al., 2001; Wang et al., 2008]).
For example, some reports suggested immune dysfunction and/or generalized inflammation were to blame for CFIDS- patients were noted to have aberrant populations of T cells, B cells, and natural killer cells, and altered patterns of inflammatory cytokine expression (Devanur and Kerr, 2006). Therefore treatment was initiated with immunoglobulins to eliminate rogue autoantibodies; antihistamines to inhibit the allergic responses; interferons and tumor necrosis factor inhibitors to inhibit wholesale the immune response; and non-steroidal anti-inflammatories to reduce inflammation- yet none of these treatments produced consistent results (perhaps unsurprisingly, as the original immunopathology reports were themselves, in retrospect, rather equivocal) (Devanur and Kerr, 2006; Prins et al., 2006). Abnormalities in endocrine function were also observed. In particular, there was a consistent hyporesponsiveness in CFIDS patients of the hypothalamic-pituitary-adrenal axis (HPA), possibly leading to abnormal stress and immune responses in these individuals. However, treatment with exogenous corticosteroids (for example, hydrocortisone), had no consistent effect (Afari and Buchwald, 2003). Depression was once considered a possible cause of CFIDS (although it no longer is) and was treated with tricyclic antidepressants and selective serotonin reuptake inhibitors, with no consistent effect (Afari and Buchwald, 2003). Bacterial infection was also explored as a cause. For example, a significant number of patients developed chronic fatigue syndrome post-Lyme disease or Q
fever, both of which have bacterial etiologies (Treib et al., 2000; Ledina et al., 2007). However, treatment with a variety of broad-spectrum antibiotics had no consistent effect (Afari and Buchwald, 2003). Finally, a substantial body of evidence suggested that persistent viral infection, most likely with the Epstein Barr Virus or with an enterovirus, was responsible for CFIDS. Most convincingly, a significant proportion of CFIDS patients report a period of flu-like illness preceding the onset of fatigue, and stress, which can reactivate latent viral reservoirs, was identified as a predisposing factor for CFIDS. Yet antiviral treatment, as others, had no consistent effect (Prins et al., 2006; Afari and Buchwald, 2003).
The only effective treatments thus far have been cognitive behavioral therapy (CBT) and graded exercise therapy (GET). CBT is a counseling-based intervention that teaches patients to take control over CFIDS by explaining the current medical understanding of CFIDS, encouraging a change in patients fatigue-associated thoughts and behaviors, and promoting a gradual return to physical activity. CBT has been effective in reducing CFIDS symptoms in about 70% of patients (Prins et al., 2006). In contrast to CBT, GET focuses only on a gradual increase in physical activity, with little attention paid to cognition. GET has been successful in reducing CFIDS symptoms in 55% of patients (Prins et al., 2006). Pacing, or adjusting the intensity of daily activities to match energy levels, is advocated by CFIDS patient organizations as another effective treatment, but this has yet to be tested empirically (Prins et al., 2006; White et al., 2007).
Unfortunately, the success of such psychological treatments as CBT and GET has only reinforced the stereotype that CFIDS is a purely psychiatric disease (Prins et al., 2006). Also
reinforcing this stereotype is the observation that predisposing factors for CFIDS include personality traits such as neuroticism and introversion, while other predictors of poor response to treatment are such psychological factors as stress, a belief in a physical cause of the illness, a strong focus on symptoms, and a poor sense of control over symptoms (Afari and Buchwald, 2003). Yet basic research has continues to indicate that physical pathological processes are occurring in CFIDS patients (see below).
Aside from CBT and GET, CFIDS treatment is symptomatic and supportive, and regardless of the therapy chosen, total recovery is rare. Although many patients experience some improvement with therapy, residual symptoms are common, and relapses may occur throughout life (Prins et al., 2006; Priebe et al, 2008).
The future of chronic fatigue immune dysfunction syndrome
Thankfully, in recent years the medical community has become more accepting of CFIDS as a physical disease process, which has prompted renewed scientific interest in this disease and has produced a spate of findings which add to the understanding of this disease as a complex, multi-system disorder. For example, abnormal thermoregulation in teenagers with CFIDS suggested the disease may impair normal sympathetic nervous function (Wyller et al., 2007), while fMRI observations suggested that CFIDS patients may have an abnormally-functioning anterior cingulated cortex- a part of the brain responsible for motivation (de Lange et al., 2004). Other authors reported dysfunctional central serotonin metabolism (Narita et al., 2003). Alterations in muscle tissue have also been observed, with a reportedly abnormal preponderance of fast-twich fibres in CFIDS patients (Pietrangelo et al., 2009). Altered urinary output of some metabolites,
including asparagines, phenylalanine, branch chain amino acids, tyrosine, and others, suggested that CFIDS patients suffer from quantifiable metabolic derangements (Afari and Buchwald, 2003). Significant changes in composition of gut microflora have been observed in CFIDS patients, suggesting a gastrointestinal origin for the syndrome (Sheedy et al., 2009; Evengard et al., 2007). Finally, some twin studies suggested a heritable component to CFIDS (Afari and Buchwald, 2003). These and other results indicate that CFIDS truly is a whole-body disease.
Work to identify genetic and protein biomarkers is also ongoing and may soon improve ability to accurately diagnose CFIDS. For example, single nucleotide polymorphisms in genes involved in glucocorticoid metabolism, serotonin pathways, and nervous signal transduction have all been linked to CFIDS, while microarray studies have implicated a broad set of genes differentially-expressed in CFIDS patients (Goertzel et al., 2006; Fang et al., 2006). Interestingly, Kerr et al. (2007) have shown four genes of unknown function with highly significant associations to CFIDS, suggesting that our current genetic net may as yet be cast too narrowly to identify important CFIDS genes. Protein biomarkers of CFIDS have been identified as well, in blood and cerebrospinal fluid (Kerr et al., 2007; Baraniuk et al., 2005).
Most importantly, a new conceptual framework for CFIDS is emerging that may improve treatment of the syndrome. In brief, CFIDS seems most likely to result from one of several infectious etiologies causing persistent, low-level immune dysregulation and subsequent HPA dysfunction via cytokines that span the immune/endocrine gap (for example, IL-1 and IL-6) (Prins et al., 2006; Afari and Buchwald, 2003). This occurs on a background of environmental (i.e. stress) and genetic predisposing factors. This framework is useful because it allows
researchers to legitimately investigate CFIDS without requiring the identification of a single etiological agent. It also eschews the idea that a single treatment modality will successfully treat CFIDS, instead allowing that multiple, personalized treatment options specific for particular infectious, immune, and endocrine etiologies may be more effective. Finally, it acknowledges the complex, long-term process that is likely responsible for CFIDS. This last will hopefully further the acceptance of CFIDS by the medical community and society at large as it more appropriately conceptualizes the disorder as a multifactorial disease whose pathogenesis will be, as a result, extremely difficult to explain.
References
Afari, N., and Buchwald, D. Chronic fatigue syndrome: A review. American Journal of Psychiatry 2003, 160:221-236.
Anderson, J.S. and Ferrans, C.E. The Quality of Life of Persons with Chronic Fatigue Syndrome. The Journal of Nervous and Mental Disease 1997, 185:359-367.
Arroll, M.A. and Senior, V. Individuals experience of chronic fatigue syndrome/myalgic encephalomyelitis: An interpretative phenomenological analysis. Psychology & Health 2008, 443-458.
Asbring, P. and Narvanen, A.L. Ideal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgia. Social Science and Medicine 2003, 57:711-720.
Asbring, P. and Narvanen, A.L. Womens experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qualitative Health Research 2002, 12: 148-160.
Baraniuk, J.N., Casado, B., Maibach, H., Clauw, D.J., Pannell, L.K., and Hess , S. A chronic-fatigue syndrome-related proteome in human cerebrospinal fluid. BMC Neurol 2005, 5: 22.
Bentall, R.P., Powell, P., Nye, F.J., and Edwards, R.H.T. Predictors of response to treatment for chronic fatigue syndrome. Br J Psychiatry 2002, 181: 248-252..
Buchwald, D., Pearlman, T., Umali, J, Schmaling, K., and Katon, W. Functional status in patients with chronic fatigue syndrome, other fatiguing illnesses, and healthy individuals. American Journal of Medicine 1996, 101:364-370.
Carruthers, B.M., Jain, A.K., De Meirleir, K.L., Peterson, D.L.., Klimas, N.G., Lerner, A.M., Bested, A.C., Flor-Henry, P., Joshi, P., Powles, A.C.P., Sherkey, J.A., and van de Sande, M.I. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. Journal of Chronic Fatigue Syndrome 2003, 11:7-116.
Cairns, R. and Hotopf, M. A systematic review describing the prognosis of chronic fatigue syndrome. Occupational Medicine 2005, 55:20-31.
Craig, T. and Kakumanu, S. Chronic Fatigue Syndrome: Evaluation and Treatment. American Family Physician 2002, 65:1083-1090.
Devanur, L.D. and Kerr, J.R. Chronic fatigue syndrome. Journal of Clinical Virology 2006, 37: 139-150.
De Lange, F.P., Kalkman, J.S., Bleijenberg, G., Hagoort, P., vd Werf, S.P., van der Meer, J.W.M, and Toni, I. Neural correlates of the chronic fatigue syndrome- an fMRI study. Brain 2004, 127:1948-1957.
Edwards, C.R., Thompson, A.R., and Blair, A. An overwhelming illness- Womens experiences of learning to live with chronic fatigue syndrome/myalgic encephalomyelitis. Journal of Health Psychology 2007, 12:203-214.
Evengard, B., Nord, C.E., and Sullivan, A. Patients with chronic fatigue syndrome have higher numbers of anaerobic bacteria in the intestine compared with healthy subjects. International Journal of Antimicrobial Agents 2007, 29: S340-S340.
Fang, H., Xie, Q., Boneva, R., Fostel, J., Perkins, R., and Tong, W. Gene expression profile exploration of a large dataset on chronic fatigue syndrome. Pharmacogenomics 2006, 7: 429-440.
Fukuda, K., Sstraus, S.E., Hickie, I., Sharpe, M.C., Dobbins, J.G., Komaroff, A., the International Chronic Fatigue Study Group. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med 1994, 121:953-959.
Gilje, A.M., Soderlund, A., and Malterud, K. Obstructions for quality care experienced by patients with chronic fatigue syndrome (CFS)- A case study. Patient Education and Counseling 2008, 73: 36-41.
Goertzel, B.N., Pennachin, C., de Souza Coehlo, L., Gurbaxani, B., Maloney, E.M., and Jones, J.F. Combinations of single nucleotide polymorphisms in neuroendocrine effector and receptor genes predict chronic fatigue syndrome. Pharmacogenomics 2006, 7: 475-483.
Gonzales, R. and Nadler, P.L. Fatigue and Chronic Fatigue Syndrome. In: McPhee, S.J., Papadakis, M.A., and Tierney, L.M., Jr., editors. Current Medical Diagnosis and Treatment 2009. United States of America: The McGraw Hill Companies; 2009.
Jason, L.A., Fennell, P.A., and Taylor, R.R. Handbook of Chronic Fatigue Syndrome. Hoboken, New Jersey: John Wiley and Sons; 2003. 33p.
Kerr, J.R., Christian, P., Hodgetts, A., Langford, P.R., Devanur, L.D., Petty, R., Burke, B., Sinclair, L.I., Richards, S.C.M., & other authors. Current research priorities in chronic fatigue syndrome/myalgic encephalomyelitis: disease mechanisms, a diagnostic test and specific treatments. Journal of Clinical Pathology 2007, 60: 113-116.
Ledina, D., Bradaric, N., Milas, I., Ivic, I., Brncic, N., and Kuzmicic, N. Chronic fatigue syndrome after Q fever. Medical Science Monitor 2007, 13: CS88-CS92.
Malouff, J.A., Thorsteinsson, E.B., Rooke, S.E., Bhullar, N., and Schutte, N.S. Efficacy of cognitive behavioral therapy for chronic fatigue syndrome: A meta-analysis. Clinical Psychological Review 2008, 28: 736-745.
Narita, M., Nishigami, N, Narita, N., Yamaguti, K., Okado, N., Watanabe, Y., and Kuratsune, H. Association between serotonin transporter gene polymorphism and chronic fatigue syndrome. Biochemical and Biophysical Research Communications 2003, 311: 264-266.
Pietrangelo, T., Toniolo, L., Paoli, A., Fulle, S., Puglielli, C., Fano, G., and Reggiani, C. Functional characterization of muscle fibres from patients with chronic fatigue syndrome: case-control study. Int J Immunopathol Pharmacol 2009, 22:427-436.
Priebe, S., Fakhoury, W.K.H., and Henningsen, P. Functional Incapacity and Physical and Psychological Symptoms: How They Interconnect in Chronic Fatigue Syndrome. Psychopathology 2008, 41:339-345.
Prins, J.B., van der Meer, J.W.M., and Bleijenberg, G. Chronic Fatigue Syndrome. Lancet 2006, 367:346-355.
Raine, R., Carter, S., Sensky, T., and Black, N. General practitioners perceptions of chronic fatigue syndrome and beliefs about its management, compared with irritable bowel syndrome: qualitative study. BMJ 2004, 328: 1354-1357.
Ranjith, G. Epidemiology of chronic fatigue syndrome. Occupational Medicine 2005, 55:13-19.
Sheedy, J.R., Wettenhall, R.E.H., Scanlon, D., Gooley, P.R., Lewis, D.P., McGregor, N., Stapleton, D.I. Butt, H.L., and De Meirleir, K.L. Increased D-Lactic Acid Intestinal Bacteria in Patients with Chronic Fatigue Syndrome. In Vivo 2009, 23: 621-628.
Travers, M.K. and Lawler, J. Self within a climate of contention: Experiences of chronic fatigue syndrome. Social Science & Medicine 2008, 66:315-326.
Treib, J., Grauer, M.T., Haass, A., Langenbach, J., Holzer, G., and Woessner, R. Chronic fatigue syndrome in patients with Lyme borreliosis. European Neurology 2000, 43:107-109.
Wang, T.F., Zhang, Q.H., Xue, X.L., and Yeung, A. A systematic review of acupuncture and moxibustion treatment for chronic fatigue syndrome in China. American Journal of Chinese Medicine 2008, 36:1-24.
Wessely, S., Nimnuan, C., and Sharpe, M. Functional somatic syndromes: one or many? Lancet 1999, 354:936-939.
White, P.D., Sharpe, M.C., Chalder, T., DeCesare, J.C., and Walwyn, R. Protocol for the PACE trial: A randomized controlled trial of adaptive pacing, cognitive behaviour therapy, and graded exercise as supplements to standardized specialist medical care versus standardized specialist medical care alone for patients with the chronic fatigue syndrome/myalgic encephalomyelitis or encephalopathy. BMC Neurology 2007, 7: 6.
Whiting, P., Bagnall, A.M., Sowden, A.J., Cornell, J.E., Mulrow, C.D., and Ramirez, G. Interventions for the treatment and management of chronic fatigue syndrome: A systematic review. JAMA 2001, 286: 1360-1368.
Wyller, V.B., Godang, K., Morkrid, L., Saul, J.P., Thaulow, E., and Walloe, L. Abnormal thermoregulatory responses in adolescents with chronic fatigue syndrome: relation to clinical symptoms. Pediatrics 2007, 120: 129-137.